Everything parents need to know about food allergies in babies
Updated Jan 02, 2026

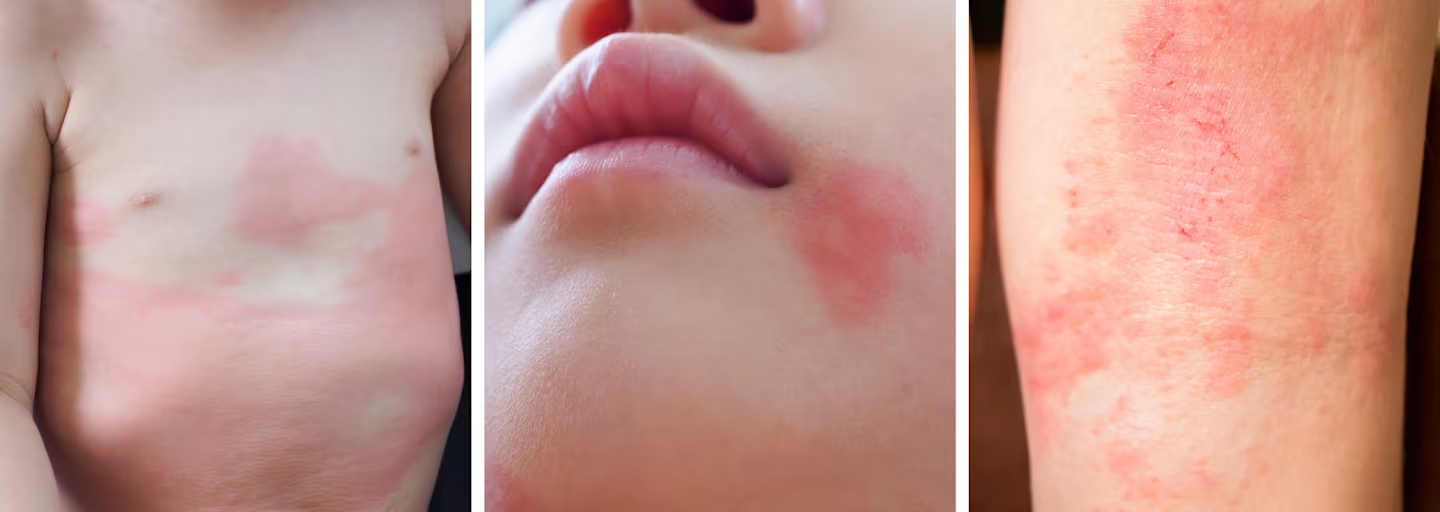
Editor's note: Photos in this article contain examples of food allergies on babies which some may consider sensitive subject matter.
About 7.6% (roughly 5.6 million) of children in the U.S. have a food allergy, according to a 2018 report published in the journal Pediatrics []. Of those affected, about 40% have more than one allergy. The most common food allergies among children are peanut, cow’s milk, and shellfish. Many children outgrow their food allergies in early childhood, but some do not.
Below you will find basic information about food allergies including their causes, signs, and symptoms, plus how to prevent them. However, food allergies differ from child to child and it’s best to work closely with your pediatrician or an allergist to determine your baby’s risk and need for testing or treatment.
What causes food allergies in babies?
Food allergies happen when the body’s immune system mistakes a protein in food as harmful and tries to fight it off. The immune response causes the common signs and symptoms associated with allergies.
While the exact cause of food allergies [] is unknown, they do tend to run in families and people with eczema, asthma, or hay fever are more likely to develop food allergies. The first signs of a food allergy usually occur in childhood, but they can develop at any age.
How to tell if a baby is allergic to food? Signs and symptoms
Symptoms of a food allergy range from mild to severe, and the severity of previous reactions [] does not predict future reactions. An allergic reaction may involve the skin, the digestive system, the cardiovascular system, or the ability to breathe.
According to the American Academy of Pediatrics [], the following are common signs and symptoms of food allergies:
How fast do food allergies appear in babies?
Food allergy reactions are highly variable and may be different every time your baby is exposed to the trigger food. However, many reactions occur quickly after consuming the food in question.
Symptoms often appear minutes after ingestion and most commonly appear within two hours. In some rare cases, a reaction may take four to six hours or longer to appear.
How long do food allergies last in babies?
Many children outgrow food allergies during early childhood. Currently, it is estimated that 80% to 90% of , , wheat, and soy allergies [] will go away by the time the child is 5 years old. Other allergies—such as , tree nuts, and seafood—are less likely to be outgrown.
It’s important to continue consulting your pediatrician or allergist to watch your child’s food allergies and test to see if they’ve outgrown them if necessary.
What does a food allergy look like in a baby?
As we mentioned above, food-related allergic reactions can show up as many different forms of symptoms, not just in regards to the skin. However, when food allergy symptoms do appear on your baby's skin, here are just a few examples of what it might look like.
Common Allergenic Foods
It’s possible to have an allergic reaction to any food, but food allergies are most commonly caused by the following:
Cow’s milk
Eggs
Peanuts
Tree nuts
Fish
Shellfish
Wheat
Soy
Sesame
In children, the most common food allergies are milk, peanuts, and shellfish.
Food allergies vs. food intolerance: what’s the difference?
While both a food allergy and food intolerance can cause unpleasant symptoms, there are a few major differences between the two.
First, a food allergy is caused by an immune system response and can be diagnosed with medical testing. Food intolerance does not cause an immune response and may be more difficult to diagnose. Food allergies tend to be more severe and require complete avoidance of the food whereas an intolerance may allow the person to consume small amounts.
Common examples of food intolerances are lactose intolerance and sensitivity to additives found in food.
Celiac disease is not characterized as a food allergy or food intolerance. It is an autoimmune condition, which requires those affected to avoid gluten in their diets.
How to test for food allergies?
If you suspect your baby has a food allergy, you should call your pediatrician right away. They will help guide you to the next steps which will likely be to see an allergist for testing.
Be prepared to answer questions about your family medical history, the symptoms your baby experienced, and how long they lasted. After that, the allergist will recommend what sort of testing, if any, is needed.
According to the American College of Allergy, Asthma, and Immunology [], the most common food allergy tests are:
Skin-prick test
During a skin-prick test, a small amount of liquid containing the allergen is placed on the arm or back. Then the skin is pricked to allow the liquid to go under the skin. If a bump, similar to a mosquito bite, develops, the test is considered to be positive.
Blood test
A blood test can be used to measure the amount of a certain antibody in the blood specific to the food being tested. It is not quite as exact as a skin test.
Oral food challenge
An oral food challenge is considered the most accurate way to make a diagnosis, but it must be completed under medical supervision. During an oral food challenge, your baby would be fed small amounts of the suspected food and observed to see if a reaction occurs.
Since there is a risk for a severe reaction, this should NEVER be completed at home.
Treatment of food allergies
The primary way to manage and treat a food allergy is to avoid the trigger food. Avoidance is the best method since allergic reactions are unpredictable and it’s not possible to know how your baby will respond to exposure. Your baby’s doctor may also prescribe an epi-pen in case of accidental exposure.
It is also helpful to learn how to read food labels including the different ways the food may be named or listed on the label. A registered dietitian can help you learn how to avoid certain foods and how to fill in any nutritional gaps.
How to protect your baby from food allergies?
Since the exact cause of food allergies is unknown and possibly genetic, it isn’t entirely possible to prevent them. The latest research and recommendation from the American Academy of Pediatrics [] provides the following information for parents looking to reduce the risk of food allergies and eczema in their children.
Exclusive breastfeeding for around 3-4 months
The research around breastfeeding and specific food allergy prevention is inconclusive. However, evidence shows breastfeeding for 3 to 4 months reduces the development of eczema for the first two years of life and any longer duration of breastfeeding may reduce asthma throughout early childhood. Both eczema and asthma have been associated with higher food allergy risk.
No allergen restriction in mother’s diet
The report [] found no evidence to support the restriction of the top allergen foods as a method to prevent allergies in one's diet while pregnant or breastfeeding.
Early introduction of allergens, especially peanut
There is currently no evidence to support delaying the introduction of the top allergens to prevent food allergies. In fact, it is recommended for most families to introduce them early, around 4 to 6 months. Research has found early introduction of peanuts helps prevent and reduce the risk of allergy [] in high-risk children.
If you have a family history of food allergies or other risk factors, it’s best to talk with your pediatrician first.
When to see a doctor
If you have a family history of food allergies or your child has a history of eczema or asthma, it is recommended to talk to your doctor prior to starting solids. They can help come up with a safe plan to introduce the top allergen foods.
If your child experiences any sort of reaction after eating a food, it’s best to call your pediatrician. Keep track of what symptoms they experienced, how long it took for a reaction to occur, and how long the symptoms lasted.
Call 911 right away if your child has severe symptoms such as trouble breathing or shows any signs of anaphylaxis [].

Takeaway
Food allergies are a serious, but manageable condition that many children outgrow during early childhood. Their exact cause is unknown, so prevention is not necessarily possible.
Every allergy is different and requires management by a medical team including your pediatrician, an allergist, and a registered dietitian. If your child experiences any signs or symptoms of a food allergy, call your doctor right away.
Share article:
Note: The content on this site is for informational purposes only and should not replace medical advice from your doctor, pediatrician, or medical professional. If you have questions or concerns, you should contact a medical professional.
10 Sources
Share article:






