A comprehensive guide to maternal mental health
Updated Jan 02, 2026

Having a baby changes your life, your hormones — even your brain []! With a precious tiny human having entered your life, it’s common to experience a range of emotions. Between learning to care for your little one, sleep deprivation, and postpartum hormone changes, the early days can be filled with highs and lows.
But even once you’re beyond the fourth trimester, motherhood can be tough as new challenges arise with each new stage of growth and development. Along the way, you’re also navigating your own mental load, milestone anxiety, rage, burnout, etc. It can feel like a lot, even with a support system in place!
Experiencing some moderate levels of stress and anxiety, especially during the first weeks postpartum and throughout your child’s first year, is to be expected. However, it can be difficult to personally determine when your symptoms have gone beyond the expected range. Thresholds vary, triggers differ, and each person has a unique response to stress. Asking for help or admitting to yourself or loved ones that you’re struggling can be really tricky, too. Plus, it can be tough to track down resources and help.
Even though 1 in 4 people [] will experience a postpartum mental health issue, perinatal or postpartum mood and anxiety disorders (PMADs) are often overlooked and underreported. In this article, we hope to help parents better understand the many ways mental health can be impacted by this milestone and share resources for support.
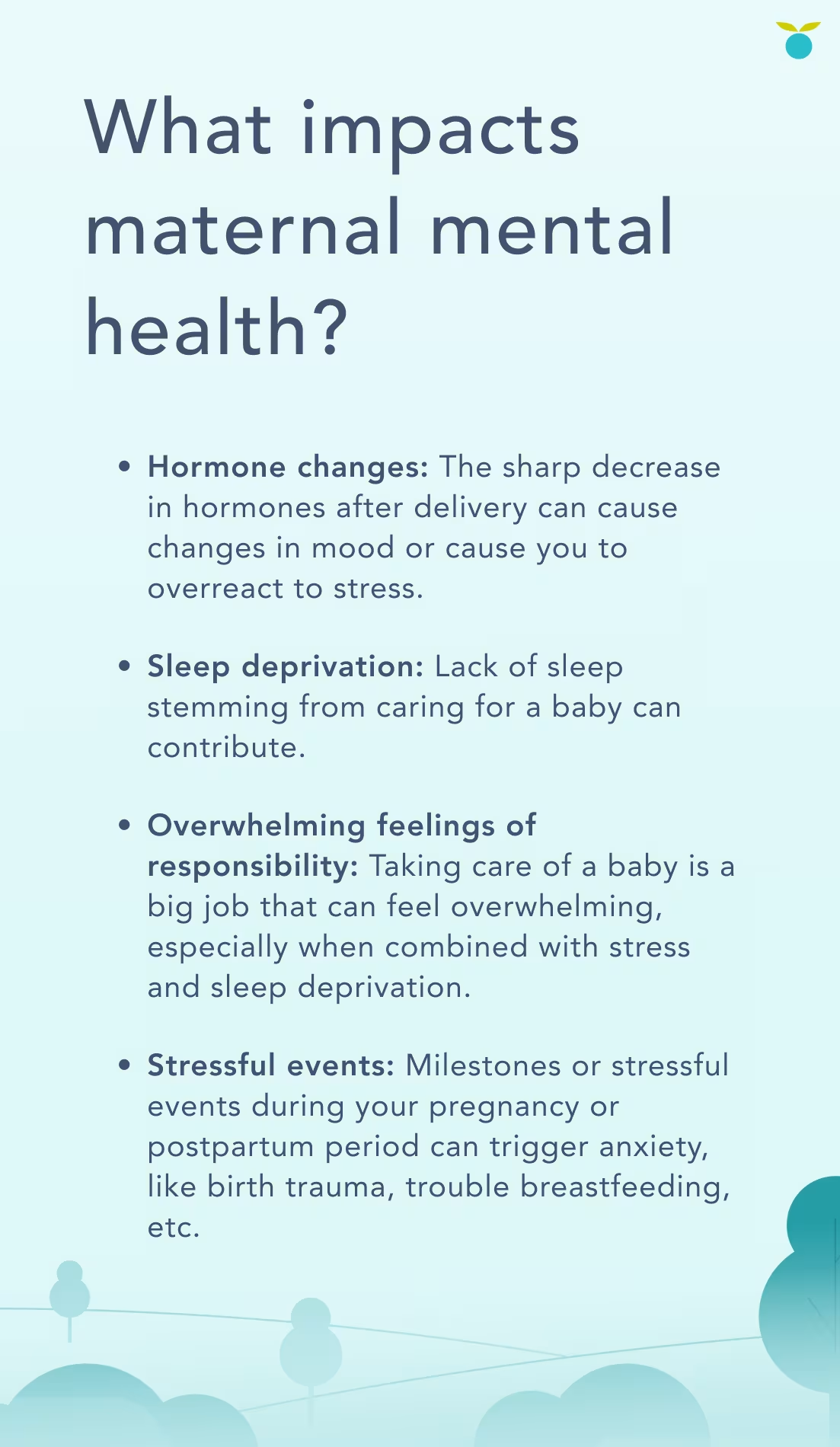
What impacts maternal mental health?
There aren’t singular causes of maternal mental health conditions, though the following factors may contribute to them.
Baby blues
The first few weeks postpartum can feel like a roller coaster of emotions. Some moments are joyous and exhilarating while others come with a flood of tears and worries. It’s normal for this phase of motherhood to feel physically and emotionally overwhelming. Most new moms (approximately 50 - 80%) [] experience what’s called “baby blues” during the first two to three weeks after giving birth. These mood swings and bouts of sadness can take some adjusting but they are a normal response to hormones shifting and typically last [] only a few days or a week or two.
While there are some similar symptoms, note that baby blues are not the same as a perinatal or postpartum mood and anxiety disorder. Some of the key differences between baby blues and PPD include the onset, severity, and duration of symptoms. A helpful way to distinguish is that baby blues normally don’t prevent a mom from caring for herself or her baby, whereas with PPD, doing basic things to take care of yourself like sleeping and eating can seem overwhelming or even impossible.

Source []
Perinatal or postpartum depression (PPD)
While temporary baby blues are common in the first few weeks of motherhood, some moms will experience a more severe, long-lasting form of depression. This is called postpartum depression and is diagnosed when at least five depressive symptoms [] are present for two weeks or longer.
While we most often hear about depression in the postpartum period, PPD is part of a larger umbrella called perinatal depression, occurring any time from the beginning of pregnancy to 12 months after a baby is born.
The CDC estimates that 1 in 8 [] new mothers experience PPD. Globally, the World Health Organization estimates 1 in 5 will experience poor mental health conditions during pregnancy. Despite its common occurrence, a 2006 study suggests up to half of PPD [] in new moms goes undiagnosed from factors like not wanting to disclose it to family members. There are many stigmas around PPD that make it difficult to talk about. Additionally, many moms may already face a lack of support for their child that makes it hard to prioritize their well-being too.
If untreated, research shows that PPD symptoms can continue for at least three years. Seeking treatment early gives moms the resources they need to manage depression, both in the postpartum period and beyond. For half of those [] who are diagnosed with PPD, it’s their first experience with having depression.

Factors that can increase risk of PPD:
Stressful pregnancy or traumatic birth
Having a premature or special needs baby
Difficulty breastfeeding
Relationship, family, or financial troubles
Having twins, triplets, or other multiples
PPD in a previous pregnancy
Source []
Postpartum anxiety (PPA)
Worrying often comes with the territory when you become a mom. However, when anxious or intrusive thoughts (i.e. unwanted thoughts of accidental harm or intentionally harming your baby) are impacting your ability to enjoy motherhood or are causing sleep and other health issues, these may be signs that something else is at play beyond typical concern for your little one.
Studies have shown PPA affects between 11% and 21% [] of people, though an exact estimate is tricky because there’s no specific diagnostic test for postpartum anxiety. Sometimes a provider will diagnose PPA during an assessment for postpartum depression.
There’s a wide spectrum for when someone may start experiencing postpartum anxiety. It can begin as early as when trying to conceive, due to factors like hormone changes, recurrent losses, or negative tests. It can also develop during pregnancy, or right after birth. Or it may not develop until your baby is a few months old.
Symptoms can include:
Source []
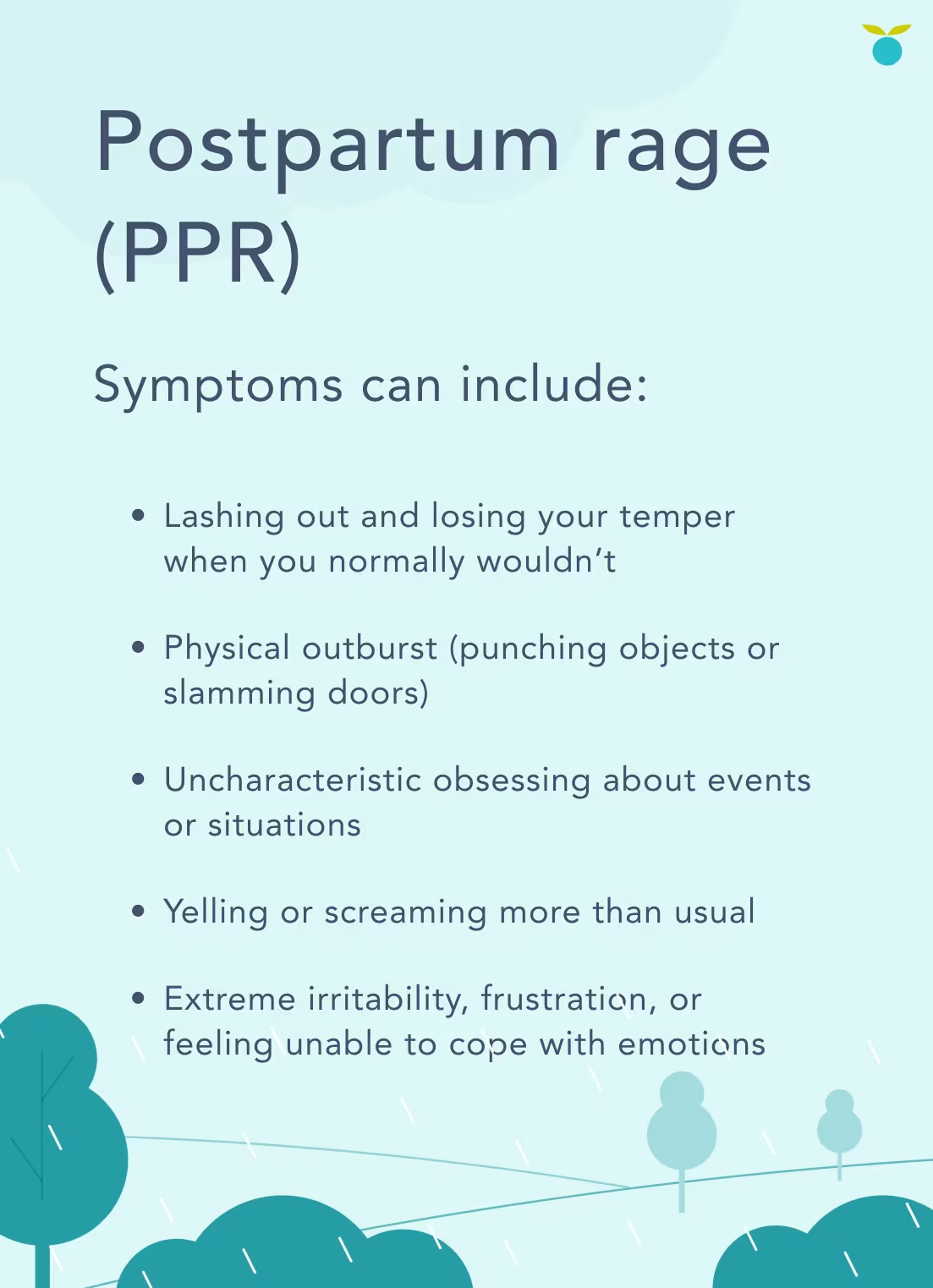
Postpartum rage (PPR)
Postpartum rage often involves pervasive anger, irritability, frustration, or losing your temper in ways that feel uncharacteristic or different from your normal baseline. Moms who struggle with PPR often wake up feeling at maximum capacity instead of experiencing bouts of anger due to a specific trigger. There’s often an underlying current of anger that permeates all facets of life, even happy moments. Postpartum rage is often a symptom of depression or anxiety and can coincide with other symptoms like hopelessness, excessive crying, and negative self-talk.
There aren’t many studies specific to postpartum rage, as it’s often folded into postpartum depression or overlooked on its own. PPR is most common within the first six weeks to one year postpartum. []
Source []
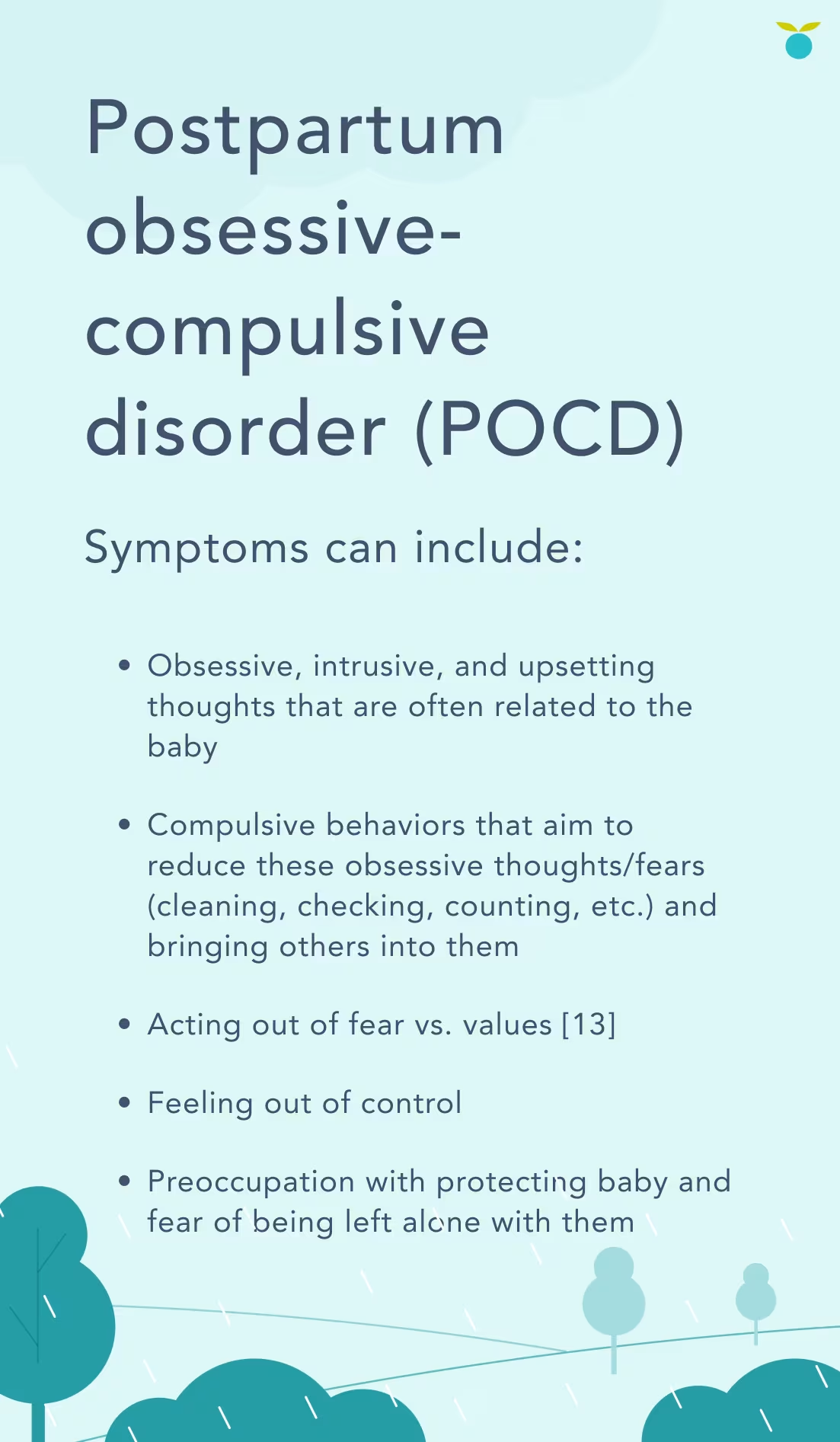
Postpartum obsessive-compulsive disorder (OCD)
Perinatal or postpartum obsessive-compulsive disorder is a type of severe anxiety disorder that involves intrusive thoughts that are followed by engaging in a compulsion or action/behavior in an attempt to alleviate the anxiety they are experiencing.
For example, an intrusive thought might be that your baby is going to stop breathing and the compulsion could be checking every few minutes to make sure they’re safe. There’s research that suggests the more you check, the less confident [] you become in your memories. Then your brain thinks checking is worthwhile, which erodes your own trust and confidence over time. When checking doesn’t soothe your anxiety, the cycle continues.
This type of OCD can occur [] during or right after childbirth or may develop 4 to 6 weeks later. It’s estimated that postpartum or perinatal OCD affects 3 - 5% of new mothers [].
Source []
Postpartum psychosis (PPP)
Postpartum psychosis is a rare and severe form of PMAD. It is considered a psychiatric emergency and should be treated immediately [] as it can lead to life-threatening thoughts or behaviors. While extreme cases are often reflected in the media, know that PPP is treatable and early intervention increases the odds of a positive outcome. Unlike many postpartum mental health conditions, PPP can be diagnosed through physical and neurological [] exams.
It’s estimated that it affects 1 in 1,000 people []. Note that diagnoses of other mental health [] conditions (bipolar disorder, schizophrenia, etc.) may increase the risk of developing postpartum psychosis. It also has a 30 - 50% recurrence risk [] for those who’ve already experienced PPP. It’s especially important to inform your healthcare provider of your mental health history in these instances.
Postpartum psychosis usually develops in the days following birth, though it can also appear up to six weeks later []. PPP symptoms can also occur within the first year of your child’s life around hormonal changes [], such as weaning from breastfeeding or your period returning.

Source []
Partners and mental health
Postpartum mental health issues most commonly affect mothers, however, men and other partners/caregivers can be impacted too. Research suggests that men also experience hormone changes when a baby is born and 1 in 10 dads [] will experience postpartum depression. Men are 50% more vulnerable [] to PPD if their partner has PPD. It’s estimated that up to 18% [] of fathers will develop an anxiety disorder at some point during pregnancy or the first year postpartum.
After your child’s first year
Perinatal and postpartum depression and anxiety can occur any time from the beginning of pregnancy to 12 months after a baby is born. However, it can sometimes persist for years if not adequately treated. And because it often goes unnoticed, understanding these conditions and their symptoms is not just relevant to those in the child’s first year of life.
For someone with a toddler experiencing these symptoms, it may be that the depression and anxiety existed during the first year and weren’t as noticeable or that something has shifted to bring it about, like changing jobs, going through relationship struggles, etc. Hormonal levels changing, such as if you wean, can sometimes impact mental health and mood and that can be a trigger as well.
Depression doesn't always have an identifiable trigger, and it can sometimes arise when we least expect it. Whether it’s a postpartum-related mental health disorder or not, it’s important to speak with a trained medical professional to receive the support you deserve.
When and how to get help for postpartum mental health disorders
It can be overwhelming to know when to speak with someone and where to start — especially while trying to keep up with your family’s needs. Additionally, one of the reasons postpartum disorders can go overlooked is the societal pressure that leads new moms to believe they should feel nothing but joy and connection with their baby. Feelings that aren’t overwhelmingly positive can instead feel shameful, leading a mom to think they should conceal or dismiss them.
Know that struggling in the postpartum period is not a reflection of parenting or your relationship with your baby. You are a good mom with or without these conditions. In fact, if you’re reading this article, you’re taking an important first step in better understanding maternal mental health.
When to seek support
If you’re feeling depressed or anxious, or think you may be experiencing any of the other postpartum or perinatal mood disorders, it’s important to talk about it with a trained professional. You don’t have to wait for a diagnosis or extreme symptoms, as it can be beneficial to have resources and support earlier on.
A good first step is contacting your primary care provider or OBGYN to schedule an appointment if:
Your baby blues symptoms become very intense or don’t go away after a couple of weeks
Symptoms of depression last more than two weeks []
You’re not able to work or do normal activities at home
You’re having trouble caring for yourself and/or your baby
If left untreated, postpartum mood disorders and PPD can last for months [] or even longer. It often leads to harsher feelings about yourself as a parent, as you may not have the energy, focus, or emotional ability to address your baby’s needs or your own. This can become a vicious cycle that can lead to intensifying feelings of depression.
While taking steps to get help may feel overwhelming, treatment for postpartum mental health conditions is often successful. It’s estimated that 80% [] with postpartum depression will recover and feel like themselves again.
What help can look like
While you’ll want to consult your medical provider or mental health professional who can take your personal medical history and specific needs into account, there are some general ways that PPD and other PMADs can be addressed.
Mental health is a really personal experience but you’re not alone in facing it. It can be overwhelming to process and know where to start, especially because every person’s idea of support can look different. In addition to talking to your doctor, here are some other helpful avenues for support:
Social support: Asking for support can be uncomfortable, especially in the beginning. But chances are your family, friends, or other people you trust want to help.
Support groups: Postpartum support groups can provide help in a comfortable setting
Support lines: has a call/text line for 24/7 support
Self-care: This is often easier said than done with small children to care for. However, trying to get enough rest, eat a balanced diet, get outside, and ask for help when needed can be beneficial for your mental health
Mental health literacy: Continuing to learn more about these conditions and read about other parents’ experiences can be a really valuable tool. Articles, , and even social content help validate and support you.
Therapy and medication are two of the most common and effective resources for mental health treatment. It can feel like a big step and it’s normal to be a little hesitant about the idea. However, there are many different avenues within these forms of treatment, and with support from trained professionals, it is often successful.
When seeking a therapist, make sure you look for a trained perinatal/maternal mental health professional. offers virtual therapy and counseling sessions. You may also use a site like to find a local therapist.
Medicine (such as antidepressants) may be prescribed to help manage symptoms of depression. Some of them can be taken while breastfeeding. Note that it may take a period of several weeks to start working before you notice a difference. Some may continue to utilize medication past the postpartum period while others may choose to taper off.
Share article:
Note: The content on this site is for informational purposes only and should not replace medical advice from your doctor, pediatrician, or medical professional. If you have questions or concerns, you should contact a medical professional.
20 Sources
Share article:




